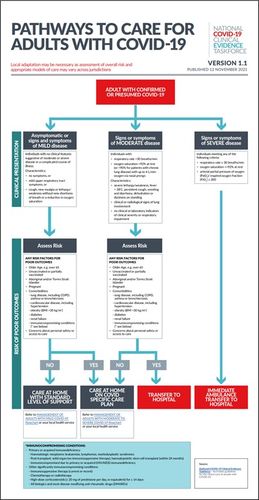
The National COVID-19 Clinical Evidence Taskforce has published a new assessment flowchart, Pathways to Care for Adults with COVID-19.
The Taskforce has also released a new recommendation on the use of pulse oximeters
In anticipation of the increasing number of people who will be treated in the primary care setting, the Primary and Chronic Care Panel, in consultation with the Guidelines Leadership Group has made a new consensus recommendation on the use of pulse oximeters:
People with risk factors for deterioration, who are being cared for at home, should be offered monitoring of oxygen saturation with pulse oximetry.
For guidance on when to escalate care, please refer to the Pathways to Care Flowchart.
Risk factors for deterioration* include:
• Older age, e.g. over 50 years for Aboriginal and Torres Strait Islander people, or otherwise over 65 years
• Unvaccinated or partially vaccinated
• Pregnant
• Concerns about personal safety or access to care
• Comorbidities: lung disease, including COPD, asthma or bronchiectasis; cardiovascular disease, including hypertension; obesity (BMI >30 kg/m2); diabetes; renal failure; immunocompromising conditions (** see below)
Use pulse oximetry with adults to assist in assessing and monitoring the severity of respiratory symptoms and detect early deterioration. Provide patients with education on how to self-monitor using pulse oximetry and when to call a GP or triple 0.
Be aware that different pulse oximeters have different specifications, and that some can under or overestimate readings especially if the saturation level is borderline. Overestimation has been reported in people with darker skin.
*The evidence enabling us to rank risk factors in order of priority is not yet available.
**Immunocompromising conditions:
• Primary or acquired immunodeficiency:
• Haematological neoplasms: leukaemias, lymphomas, myelodysplastic syndromes
• Post-transplant: solid organ (on immunosuppressive therapy), haematopoietic stem cell transplant (within 24 months)
• Immunocompromised due to primary or acquired (HIV/AIDS) immunodeficiency
• Other significantly immunocompromising conditions:
• Immunosuppressive therapy (current or recent)
• Chemotherapy or radiotherapy
• High-dose corticosteroids (≥20 mg of prednisone per day, or equivalent) for ≥14 days
• All biologics and most disease-modifying anti-rheumatic drugs (DMARDs)

Get unlimited access to hundreds of ACP's top courses for your professional development.
Join Now